Despite their many health benefits, all sports carry the risk of overusing certain parts of the body, which can lead to injuries. Due to their close contact nature, contact sports are notoriously high risk activities when it comes to injuries. Grappling arts, that involve or focus on controlling the opponent by grabs and weight tend to show a predictable pattern of damage. Having basic knowledge of how to approach these injuries is important for getting proper care and supporting recovery, because poor healing can lead to recurring issues or a snowball effect.
In contact sports like football or rugby, athletes are more likely to experience trauma or concussions, which can carry the danger of brain injury. In grappling arts, however, practitioners are more likely to injure their joints. When fighters grab and control their opponents, they can unintentionally force a joint into an abnormal rotation. The goal of this article is to summarize the most common injuries seen in the context of grappling disciplines.
Muscle strains
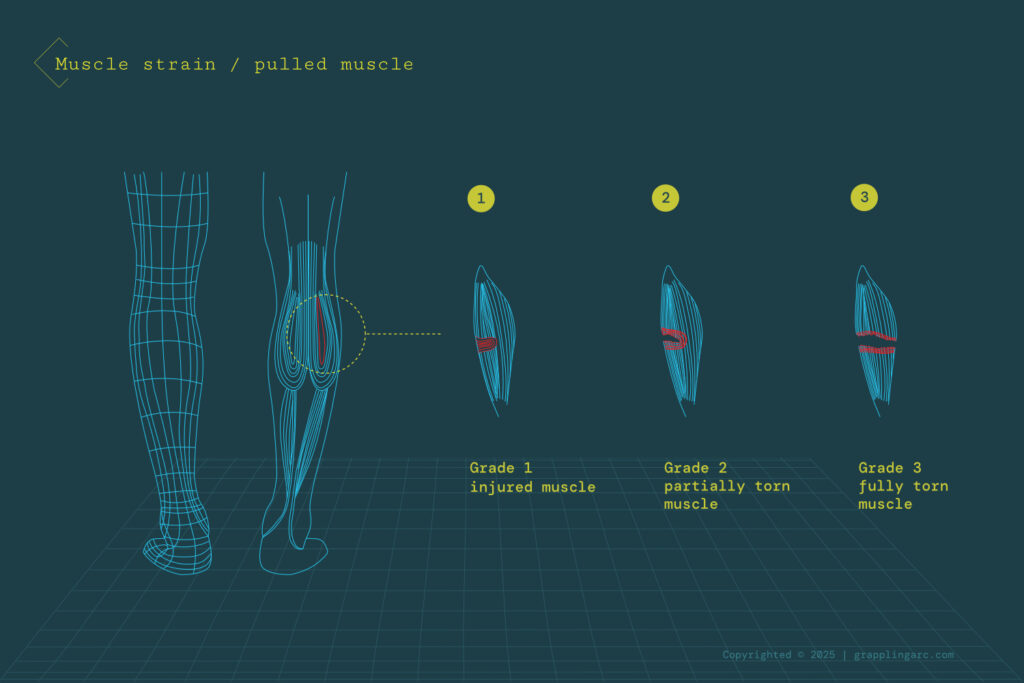
A muscle strain, also known as a pulled muscle, is a common injury that can happen to any muscle. It occurs when the muscle is stretched beyond its limit, putting excessive stress on the muscle fibers. In some cases, this can lead to a partial or complete muscle tear. A strain may happen suddenly, for example, from a direct hit during training, which usually comes with immediate pain. But it can also develop gradually when repetitive movements keep overstretching the muscle, causing the muscle or tendon to weaken over time. In some situations, the strain can also affect the tendon that connects the muscle to the bone.
Muscle strains are classified into Grade 1, Grade 2, and Grade 3. Where Grade 1 strains are the most common, while Grade 3 strains are the most severe and may require surgery to reattach the muscle.
Potential causes:
- Muscle tightness due to an inadequate warm-up before exercising
- Trying to do too much, too quickly during a workout
- A direct hit to the muscle
- Repeated overuse of the muscle
Usual symptoms:
- Swelling in the affected area
- Pain
- Tenderness
- Bruising
- Muscle spasms and weakness
Suggested treatment
For lower-grade strains, it is common to improve with home treatment alone, without any medical intervention. The standard protocol to treat a strain after an injury is known as the R.I.C.E. method (Rest, Ice, Compression, Elevation).
- Rest: Resting the muscle is the first step. Avoid any physical activity or movement that uses the injured muscle and causes pain or discomfort in the following days.
- Ice: Applying cold therapy immediately after an injury can help reduce swelling and pain. It is recommended to apply an ice pack to the affected muscle for 15–20 minutes every 2–3 hours. Wrap the ice pack in a cloth to protect your skin.
- Compression: Lightly wrap the injured area with a compressive bandage. This helps reduce swelling and stabilizes the body part. However, the bandage should not be too tight, as it may restrict proper blood flow.
- Elevation: Elevating the injured body part can decrease blood flow to the area and reduce swelling.
Over-the-counter pain relievers and nonsteroidal anti-inflammatory drugs (NSAIDs) can also be used to reduce pain and swelling. Special exercises may be provided by a physical therapist or through online physiotherapy programs to aid in recovery. After this first acute stage, sports massage can help eliminate scar tissue in the muscle and keep the muscle flexible. Because car tissue can trap the nerves and cause pain, proper recovery and caution is essential, an injured muscle is highly susceptible to reinjury.
Knee sprains
The knee is the most commonly injured part of the lower body in grappling arts. A knee sprain is an injury that affects the ligaments that stabilize the joint and connect the bones. The injury is often accompanied by a popping sound and can cause the leg to buckle when you try to stand on it. Swelling and typically severe pain may develop in the following one to two days.
The knee is a relatively complex structure, with four ligaments and multiple muscles intertwined with nerves. The Anterior Cruciate Ligament (ACL) is the most frequently injured, followed by the Medial Collateral Ligament (MCL). In contact sports, the ACL is most commonly injured due to sudden stops or changes in direction while attacking or passing guard. Grapplers can also injure their ACLs during leg locks when the joint is bent at unnatural angles.
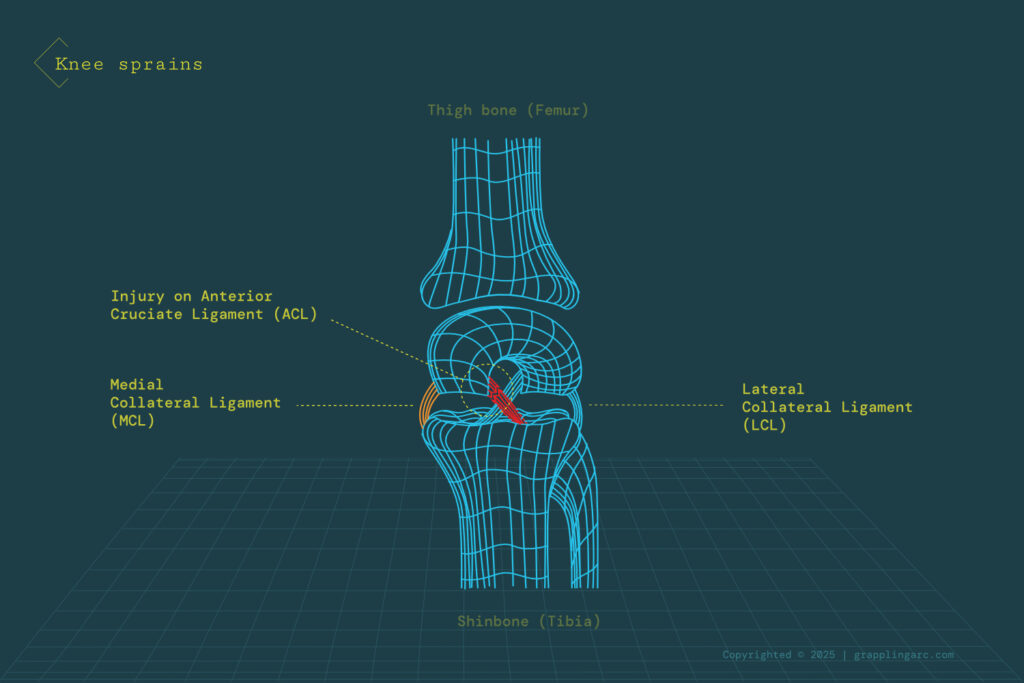
Knee sprains can also be categorized into three grades: Where Grade 1 is a mild injury with a stretched ligament, Grade 2 involves a partial tear, and Grade 3 is a complete rupture of the ligament.
Usual symptoms:
- Severe pain
- Swelling or bruising
- Limited range of motion in the knee
- Popping sensation in the knee
- Instability
- Knee may appear deformed
Suggested treatment
It is recommended to use the earlier described R.I.C.E method for first aid immediately after an injury in order to prevent it from getting worse. Over-the-counter pain killers and nonsteroidal anti-inflammatory drugs (NSAIDs) can be added when swelling appears, which is usually after one to two days.
However, if there is no improvement within two weeks, you should seek medical attention for a proper diagnosis and treatment plan. In this case, the severity of the tear and the exact ligament, or potentially other damaged tissues, require a detailed examination and possibly imaging/scanning. Based on the results, a doctor can recommend a rehabilitation program, which can begin once swelling and bruising have reduced, typically with the assistance of a specialized physical therapist or online knee exercise program. The received injury-specific exercises help to restore the knee’s range of motion.
Severe cases, such as Grade 3 injuries, may require surgical intervention, especially for professional athletes where regaining full range of motion is essential to continue their careers.
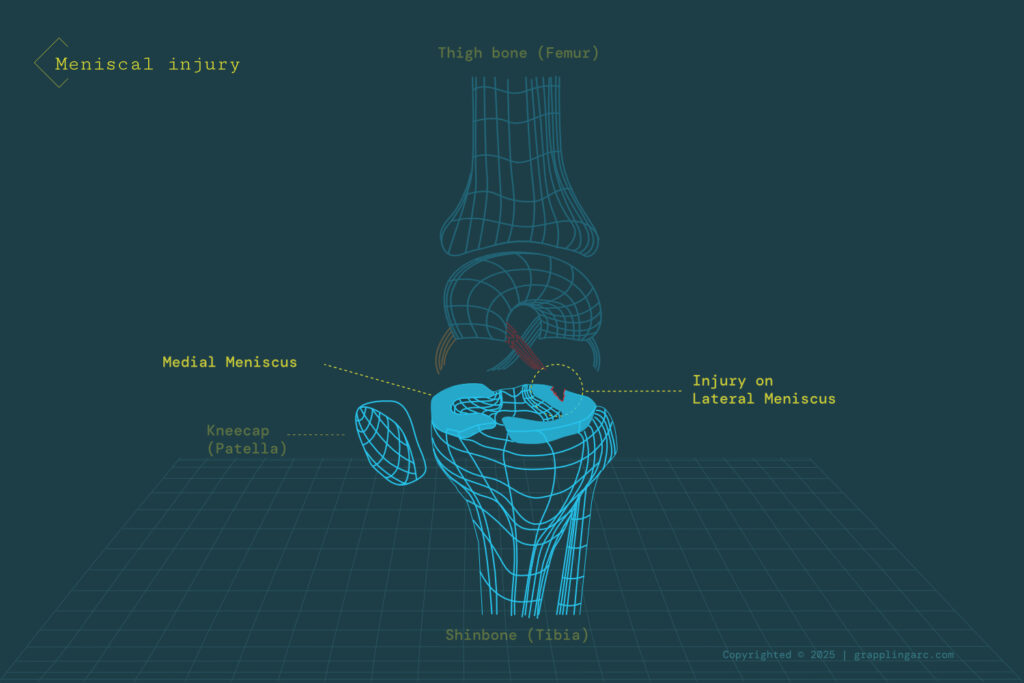
Meniscal Injury
The meniscus is a cartilage in the knee that acts as a cushion between the bones. It is quite prone to tearing in contact sports, usually caused by jumping, especially with speed and weight, such as during guard passes and takedowns in grappling training. Meniscus injuries can also occur during any activity that forcefully twists or rotates the knee, particularly when the full body weight is on it.
Usual symptoms:
- Moderate to severe knee pain, especially during twisting or rotating motions
- Swelling or stiffness
- Knee locking in position
- Difficulty bending or fully extending the knee
Suggested treatment
The R.I.C.E. method described earlier is the recommended initial treatment for the injury. The swelling can take 24 hours to appear, taking medication before that is not recommended. Medical attention is needed only if symptoms do not improve within one to two weeks. At that point, it is worth visiting a doctor for a proper assessment. In many cases, physical therapy is sufficient to reduce stress on the knee, improve range of motion, and strengthen the surrounding muscles to protect the area.
However, the self-healing capacity of cartilage is very limited because it lacks its own blood supply. If the tear is severe or there is a loose fragment of the meniscus causing other problems, surgery may be required.
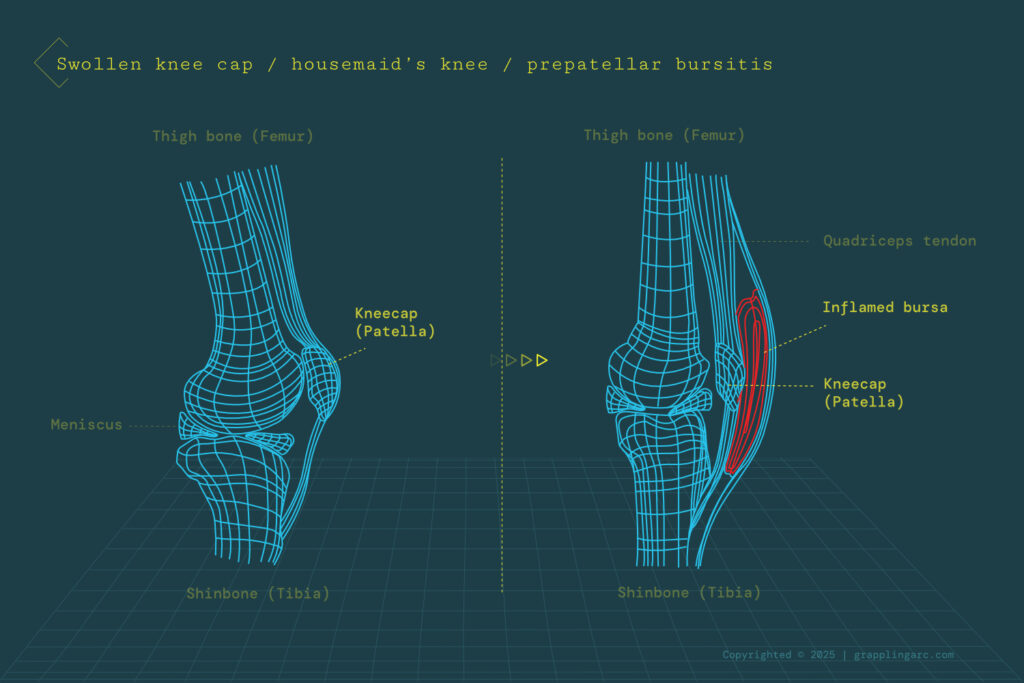
Swollen knee cap (Prepatellar bursitis)
Prepatellar bursitis, often called ‘housemaid’s knee,’ can occur when the knee receives repeated direct impacts on the kneecap from regular kneeling or falling. The bursa, which becomes swollen, is a small fluid-filled sac that acts as a protective cushion for the joint. Regular irritation of the bursa causes it to swell, and the extra fluid puts pressure on other parts of the knee.
Usual symptoms:
- Noticeable knee swelling; knee may appear deformed
- Limited range of motion
- Pain (not always present)
Suggested treatment
Patella’s bursitis is usually a minor injury and disappears with enough rest. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce swelling and discomfort. If swelling persists after following the R.I.C.E. method for one to two weeks, a doctor may recommend corticosteroid injections.
Fever and red colouring in the swelling area indicate a bacterial infection, likely due to an open wound in the knee. This requires immediate medical treatment and it’s highly recommended that you visit the nearest emergency department or hospital in this case.
Ankle sprain
Ankle sprains are another common injury among wrestlers and grapplers. Like knee sprains, they affect the ligaments that hold the ankle bones together. The injury has similar symptoms to a knee sprain, including swelling and limited range of motion. This type of injury usually results from twisting the ankle in abnormal positions, planting the foot the wrong way during a fight, or stepping on the opponent and losing balance.
Suggested treatment
Just as with a knee sprain, the first aid treatment would be the R.I.C.E method. After the swelling reduced, physiotherapy can be utilized to improve the ankle condition and help to regain its strength and complete range of motion.
If the ankle does not improve within one to two weeks, you should see a doctor. The doctor may recommend using crutches or a supportive bandage to reduce stress on the ankle. In severe cases, a cast may be applied to immobilize the ankle while the ligament heals. Once the restriction is removed, a specific physical therapy program or online ankle exercise program can help build the muscles back and improve mobility.
Surgery also can be a viable treatment option in severe cases, particularly for professional athletes who likely will place the ankle under further pressure.
Shoulder and elbow dislocations
A dislocation occurs when a bone pops out of its socket. In grappling arts such as wrestling, Brazilian Jiu-Jitsu, or other fight sports with grappling components like mixed martial arts, shoulders and elbows have just as high dislocation risk as the finger have.
Dislocations can happen due to the extreme pressure these joints endure during various maneuvers or falls. Depending on the severity, a dislocation can also injure the tendons, ligaments, nerves, blood vessels, and muscles around the joint, which can increase pain and cause numbness or tingling in the surrounding area.
Potential causes:
- Extreme twisting of the shoulder or elbow joint
- Forced pull or sudden impact on the joint
- Falling on the joint with body weight
Usual symptoms:
- Severe pain
- Out-of-place shoulder or elbow with visible deformity
- Inability to move the joint
- Swelling or bruising
- Numbness or tingling
Suggested treatment
It is necessary to seek immediate medical attention after a dislocation. To prevent further injury while waiting for treatment, apply ice to the area to reduce swelling and, if possible, use a splint to immobilize the joint. Because joints can dislocate in various directions and degrees, affecting surrounding tissues, only a trained professional should reposition them. Attempting to do it without proper training can cause more damage to the joint and surrounding tissues. In cases of inflammation, the doctor might administer cortisone injection as well. In severe cases, surgery might be needed to repair the joint and the tissues involved.
After the joint has been repositioned, it must be immobilized for a few days. Only after the swelling decreases should physical therapy or an online shoulder exercise program start to strengthen the muscles to prevent future dislocation. The exercises are usually performed for 8 to 10 weeks following dislocation. It is crucial to avoid putting pressure on the shoulder or elbow during the recovery period, which can take several months. When the shoulder has been dislocated, the joint is at risk of repeated dislocations, so increased awareness is necessary during training.
Cauliflower ear
Cauliflower ear, also known as a subperichondrial hematoma, is a common injury among wrestlers and gives practitioners a distinctive appearance.
It occurs when the ear suffers a heavy trauma, usually pressed to the ground or being folded during training. usually from being pressed against the mat or folded during training. The pressure causes a pocket of blood to form under the skin. As it gets bigger, the ear can fold in on itself, resulting in a noticeable deformity and, in severe cases, reduced hearing.
Usual symptoms:
- Pain
- Hearing loss
- Ear deformity
- Swelling or bruising
Suggested treatment
This condition can only be treated by a doctor. The procedure involves making a small incision in the ear to drain the accumulated blood. To prevent permanent deformity, it is recommended to seek medical attention within six hours of the injury.
References
Andrews, K., Lu, A., Mckean, L., & Ebraheim, N. (2017). Review: Medial collateral ligament injuries. Journal of Orthopaedics, 14(4), 550–554. https://doi.org/10.1016/j.jor.2017.07.017
Błach, W., Smolders, P., Rydzik, Ł., Bikos, G., Maffulli, N., Malliaropoulos, N., Jagiełło, W., Maćkała, K., & Ambroży, T. (2021). Judo injuries frequency in Europe’s top-level competitions in the period 2005–2020. Journal of Clinical Medicine, 10(4), 852. https://doi.org/10.3390/jcm10040852
Dislocated shoulder: Causes, treatment & prevention. Cleveland Clinic. (2023, May 11). https://my.clevelandclinic.org/health/diseases/17746-dislocated-shoulder
Hinz, M., Kleim, B. D., Berthold, D. P., Geyer, S., Lambert, C., Imhoff, A. B., & Mehl, J. (2021). Injury patterns, risk factors, and return to sport in Brazilian Jiu Jitsu: A cross-sectional survey of 1140 athletes. Orthopaedic Journal of Sports Medicine, 9(12), 232596712110625. https://doi.org/10.1177/23259671211062568
Mayo Clinic Staff . (2022, December 1). ACL injury. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/acl-injury/symptoms-causes/syc-20350738
Mayo Clinic Staff. (2022, August 11). Sprained ankle. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/sprained-ankle/symptoms-causes/syc-20353225
Mayo Clinic. (2022, October 11). Muscle strains. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/muscle-strains/diagnosis-treatment/drc-20450520
Patel, B., Skidmore, K., Hutchison, J., & Hatcher, J. (2023, January). Cauliflower ear. National Center for Biotechnology Information. https://pubmed.ncbi.nlm.nih.gov/29261905/
Pietrangelo, A. (2023, April 15). Muscle strains: Symptoms, causes, and prevention. Healthline. https://www.healthline.com/health/strains#_noHeaderPrefixedContent
Rishor, C., & Pozun, A. (2022, September 6). Prepatellar bursitis – statpearls – NCBI bookshelf. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK557508/
Wheeler, T. (2022, January 26). Meniscus tear in knee: Symptoms, causes, and treatments. WebMD. https://www.webmd.com/pain-management/knee-pain/meniscus-tear-injury






